Predicting COPD 1-year mortality using prognostic predictors routinely measured in primary care
C. I. Bloom ,et al.
BMC Medicine201917:73
https://doi.org/10.1186/s12916-019-1310-0
54990名の被検者 UK電子カルテ使用プライマリケアCOPDコホート
初期コホート トレーニングとtest setへ均等ランダム化割り付け
外部データは2つめのコホート
12ヶ月死亡率推定リスクモデルCox回帰でbackwards elimination使用トレーニングセット
BMI、血液検査(B)、年齢(A)、呼吸変数(気道閉塞、急性増悪)(R)、併存症使用(C)を含む80の変数具体的には・・・
FEV1, GOLD staging (FEV1 and FVC), C-reactive protein (CRP), albumin (low = < 35 g/L), haemoglobin, fibrinogen, platelets (low = < 150 × 109/L, high = > 400 × 109/L) and creatinine; creatinine above 120 μmol/L for males, or 110 μmol/L for females, was used to define chronic kidney disease (CKD). BMI was measured as kg/m2 (underweight < 19, normal = 19–25, overweight = 25–30, obese ≥ 30). Exacerbations, treated within primary (labelled as moderate) or secondary care (labelled as severe)
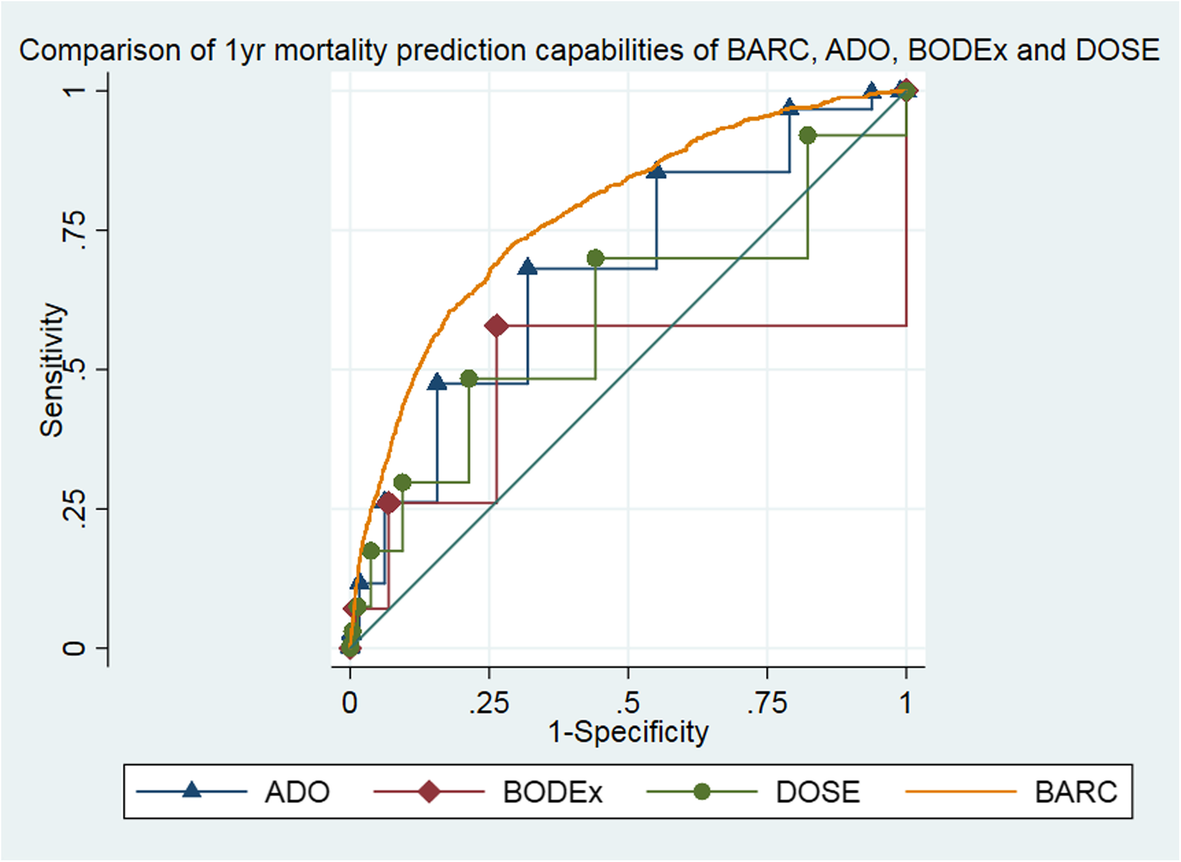
BODEx、DOSE、ADOと比較
リスクモデルでパフォーマンス推定
acceptable predictive performance
(test set: C-index = 0.79, 95% CI 0.78–0.81, D-statistic = 1.87, 95% CI 1.77–1.96, calibration slope = 0.95, 95% CI 0.9–0.99; external dataset: C-index = 0.67, 95% CI 0.65–0.7, D-statistic = 0.98, 95% CI 0.8–1.2, calibration slope = 0.54, 95% CI 0.45–0.64)acceptable accuracy predicting the probability of death
(probability of death in 1 year, n high-risk group, test set: expected = 0.31, observed = 0.30; external dataset: expected = 0.22, observed = 0.27)
BARCは既存の指数スコアよりspecialist respiratory variableなしでは優れている
(area under the curve: BARC = 0.78, 95% CI 0.76–0.79; BODEx = 0.48, 95% CI 0.45–0.51; DOSE = 0.60, 95% CI 0.57–0.61; ADO = 0.68, 95% CI 0.66–0.69, external dataset: BARC = 0.70, 95% CI 0.67–0.72; BODEx = 0.41, 95% CI 0.38–0.45; DOSE = 0.52, 95% CI 0.49–0.55; ADO = 0.57, 95% CI 0.54–0.60)